Last week’s dueling federal appeals court decisions on the legality of subsidies under the Affordable Care Act (ACA) cast – yet again – uncertainty on the future of President Obama’s health care law. Yet even as this latest case plays out, the consequences of previous legal challenges to the law are still unfolding – to some extent in surprising ways.
The Supreme Court’s decision also had a less predictable effect: It gave conservatives power to remake the Medicaid program.
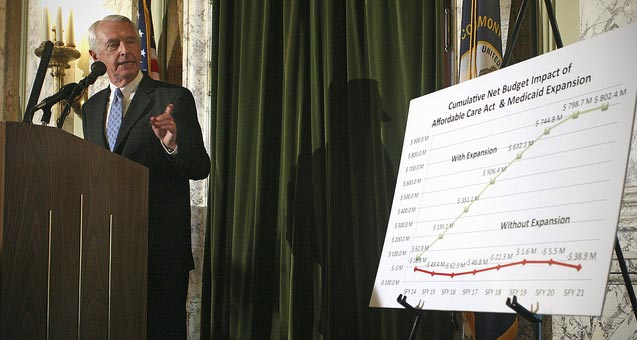
When, for instance, the Supreme Court made the ACA’s expansion of Medicaid optional for states, it was clear that this would limit the law’s reach for some time to come: Even today, some 24 states have failed to expand the program, a number that includes many of the states that need it the most. But as I’ll explore here, the Supreme Court’s decision also had a less predictable effect: It gave conservatives power to remake the Medicaid program. As Sarah Kliff of The Washington Post put it, while Obamacare is expanding Medicaid, it is ironically making it “more Republican” too.
In a still evolving story, states around the country are seeking – and obtaining – waivers from the federal government to pursue various compromise “solutions” to the Medicaid expansion, including privatization under the so-called “private option.” While the expansion of any form of Medicaid might seem like good news, there is also reason for concern. The emphasis of these plans and proposals is clear: We shouldn’t simply provide health care to those living in or near poverty. We must instead teach the poor to be better health care consumers; we must – as the noxious saying goes – give them more “skin in the game.”
How is the “private option,” together with other conservative-minded Medicaid expansions, faring in states across the nation?
Arkansas
Arkansas was the first state to obtain a “private option” Section 1115 waiver from the Centers for Medicare and Medicaid Services (CMS); this allowed it to expand Medicaid through a system in which participants receive a voucher to purchase private insurance. Despite this major concession to conservatives, the “private option” still only barely passed, and it remains (to some extent) on shaky political ground today.
The primary accomplishment of the waiver was to privatize Arkansas’ Medicaid expansion, which was no mean feat. Otherwise, as some supporters (and detractors) emphasize, it didn’t immediately change too much else. Though the most recent state survey by the Kaiser Family Foundation reported that Arkansas was planning to raise cost sharing for those under the “private option,” for now, cost sharing must be consistent with the state plan and applies only to those making more than 100 percent of the federal poverty level (FPL). But we shouldn’t be too comfortable: The latter safeguard is set to soon change.
Underlying such “innovations” is an unmistakable premise: Medicaid participants use medical care that they don’t actually need simply because it’s “free.”
Arkansas’ Medicaid legislation not only mandated the expansion of Medicaid through the private option, but also required that the state obtain waivers to establish “independence accounts” for Medicaid recipients, which would operate like health savings accounts. With these accounts, according to the law, participants would “purchase cost-effective high deductible health insurance” that would “promote independence and self-sufficiency.” These new plans will extend cost sharing under the private option to those making as low as 50 percent of the FPL (about $6,000 for an individual). A subsequent amendment to the law required that this change be effective by February 1, 2015, or end the expansion altogether.
As Michelle Andrews recently reported for Kaiser Health News, under one proposed approach to make this plan a reality, participants’ monthly payments to their health accounts (which would be run by third-party companies) would go towards paying the private plans’ deductibles and co-payments. If participants fail to meet their payments and the balance runs out, some would incur a debt to the state for unpaid co-payments for further medical services, while others (depending on income) could be refused services for failing to make a co-payment. While traditional Medicaid in Arkansas already has some co-payments, this is something new.
Underlying such “innovations” is an unmistakable premise: Medicaid participants use medical care that they don’t actually need simply because it’s “free.””We believe in consumerism,” the director of the Arkansas Department of Human Services told Andrews. By making the poor act more like consumers, “we think they’ll use care more appropriately and get a sense of how insurance works.”
It’s worth pointing out that in some parts of the world, there are no (or minimal) co-payments, deductibles or health savings accounts for everyone, much less the impoverished. That seems to work rather well. People must be different here.
Iowa and Pennsylvania
Iowa was the second state to obtain a “private option” waiver, but unlike the Arkansas waiver, it did a bit more. In addition to privatizing Medicaid for those with incomes 100 to 138 percent of FPL, the plan also instituted a monthly premium (albeit in lieu of most co-payments). But Iowa’s waiver, unlike Arkansas’, also allowed it to drop one important Medicaid benefit. For Medicaid participants with complex medical needs, it can be very difficult to arrange, coordinate and fund transportation to medical appointments, and so states have long been required to provide nonemergency medical transportation benefits to participants. Not so under the Iowa private option demonstration.
The Pennsylvania program would, like Iowa and Arkansas, privatize Medicaid.
Pennsylvania, meanwhile, is looking to follow in Iowa’s footsteps with a somewhat similar waiver application, which it had to water down considerably to have a realistic chance at CMS approval. The Pennsylvania program would, like Iowa and Arkansas, privatize Medicaid. It also seeks to increase the co-payment for nonemergency ER use. For those making above 100 percent FPL, it would impose a new premium of $25 to $35 a month (though as in Iowa this would replace many co-payments), with annual increases based on health care-specific price inflation. And in the second year of the program, consideration would be given toward implementing a premium for those making less than 100 percent FPL. As a condition of Medicaid eligibility, Governor Corbett also sought a mandatory work-search requirement for participants, but he has had to back off of this proposal in light of federal resistance to the linkage of medical benefits and job training.
Finally, concerns have been raised about reductions in benefits under the Pennsylvanian private option. Currently, Pennsylvania Medicaid has a progressive family planning benefit (the “SelectPlan for Woman”), which fully covers contraception and other reproductive health services for women making up to 185 percent FPL. Under the private option, these benefits would instead be provided by the Medicaid participants’ private insurance plan, which might actually be through their employer. In light of the Hobby Lobby decision, some state lawmakers have argued that this could result in the loss of contraceptive coverage for some Medicaid patients.
Michigan
Michigan, unlike Iowa and Arkansas, has expanded Medicaid without privatizing it, though the expansion is similarly colored by conservative health policy ideology. The Michigan expansion builds on a previous very limited waiver. In it, participants pay Michigan’s current Medicaid co-payments, while those making more than 100 percent FPL also pay contributions (2 percent of income) into health savings accounts. While it is true other states have similar co-payments to Michigan’s, the overall change that this evolving framework of co-pays, premiums and health savings accounts represents becomes clear when we note that under the traditional Medicaid program in Michigan just a decade ago, there were no co-payments or premiums for adults, whatsoever, according to a Government Accountability Office review.
It’s not about saving money, per se; it’s again about teaching participants how to be better health care consumers.
Why, one might ask, create health savings accounts for a government health care program for the poor? It’s not about saving money, per se; it’s again about teaching participants how to be better health care consumers. Health savings accounts, according to the Michigan waiver application, will help people “to become actively engaged in their health care experience” (clearly, the poor wouldn’t be interested if it was only their lives on the line). The accounts will “encourage beneficiaries to become more active consumers of their health care, to save for future healthcare expenses and become more aware of the cost of the services they receive” – as if those earning near poverty wages didn’t have enough to worry about.
Nor will things stop there: Michigan’s Medicaid legislation (page 6) directs the state health administration to obtain an additional waiver that will require those who make between 100 percent and 133 percent of FPL and who remain in Medicaid after four years to either leave Medicaid and buy private insurance, or have their cost sharing raised to 7 percent of income – with co-pays mandated at no less than 3 percent of income. Whether they obtain such a waiver from CMS remains unclear, but the overall intent – to increase cost sharing – isn’t.
Indiana
Finally, in Indiana, Gov. Mike Pence has recently submitted a waiver to CMS that follows the path of Arkansas and Iowa, but goes even further. Pence’s plan would replace traditional Medicaid via the expansion (and modification) of Indiana’s existing “Healthy Indiana Plan” (HIP), which uses high-deductible insurance provided by private insurance carriers.
Why all this complexity? Why create new or increased co-payments for people living in or near poverty, despite decades of health policy literature demonstrating that user charges deter the poor from using health care?
This rather complicated system, dubbed HIP 2.0, would be composed of two sub-plans, “HIP Plus” and “HIP Basic.” In the “HIP Plus” plan, members would be required to make monthly contributions to a “POWER” (Personal Wellness and Responsibility) account, which (the pattern here is no doubt becoming familiar) resembles a health savings account. Health care expenses would be drawn out of this account, and unspent balances could be rolled over to the following year. Monthly contributions would go as high as $25 a month, with nonpayment ultimately resulting in disenrollment from the program (at least for those making more than 100 percent FPL), together with a mandatory “lock out period” from Medicaid.
Those in “HIP Plus” who make less than 100 percent FPL and who didn’t (or couldn’t) pay the monthly contribution, would (more charitably) be downgraded to “HIP Basic” as “an alternative to disenrollment.” HIP Basic, however, has less generous benefits, as well as co-payments for all services. For comparison purposes, co-payments under the proposed HIP Basic Plan, as compared to traditional Medicaid in Indiana, are as follows:
|
Service |
Co-payment: Traditional Medicaid, 2012 |
Co-payment, proposed: HIP Basic Plan |
|
Physicians Visits |
NA |
$4 |
|
Inpatient Services |
NA |
$75 |
|
Prescriptions |
$4-$8 |
|
|
Non-emergency ER visit |
Up to $25 |
Why all this complexity? Why create new or increased co-payments for people living in or near poverty, despite decades of health policy literature demonstrating that user charges deter the poor from using health care? Why not, in other words, just expand traditional Medicaid?
Well, if we did that (according to the application for the waiver) these people would miss out on that lovely “private health insurance experience.” For HIP 2.0 will ultimately, the waiver claims, “maximize the consumerism experience” of these Medicaid participants. This “experience,” it seems (and this truly is worth quoting at length):
promotes consumerism by requiring members to make contributions into their accounts. The contributions are designed to preserve dignity among members receiving public assistance and provide them with “skin in the game,” which empowers them to demand price and quality transparency as they make cost-conscious health care decisions and take responsibility for improving their health. In addition, the infusion of market principles works to educate members and prepare them to participate in the private market . . .
Alas, such a passage takes all the fun out of trying to dissect and uncover the hidden ideological underpinnings beneath dryly-composed policy documents. But there you have it: By taking money from people who have little to no disposable income in exchange for means-tested health care, HIP 2.0 will teach the poor “consumerism” and “market principles,” help them to “preserve dignity,” and afford them (the phrase becomes only more odious with repetition) “skin in the game.”
Conclusions
In closing, it’s worth noting that some who support, and also some who oppose, these compromise expansions contend that they don’t represent major changes to the Medicaid program, or to the cost sharing burden imposed on enrollees. Now first, it should be clear that privatization alone is a deleterious change. Private insurers are far less efficient than public programs like Medicare and Medicaid. We have learned this dearly in the case of privatized Medicare (“Medicare Advantage”), which takes an estimated 13 percent in administrative costs and profit, as opposed to traditional Medicare’s approximate 2 percent overhead.
It should be clear that privatization alone is a deleterious change. Private insurers are far less efficient than public programs like Medicare and Medicaid.
And with respect to cost sharing, it’s true that changes thus far have been variable. It’s also true that Medicaid cost sharing is more of a diffuse phenomenon, one that is not restricted to red states. Some might also argue that these Medicaid co-payments and premiums look rather attractive for those who are facing much higher (and rising) deductibles and co-payments in the private insurance market (another major problem). But even small co-payments for those with little money can deter the use of necessary health care. We will see what comes of these various proposals, but the overall push toward a more “consumerist” model of Medicaid seems evident.
But how should progressives approach these privatized Medicaid expansions? A truly universal single-payer health care system would clearly be much preferable: It would eliminate altogether the need for means-tested Medicaid, which despite its benefits frequently confers inadequate access to providers and health care facilities. But until that is achieved, those with low-income need Medicaid, so how should we proceed?
It’s not an easy question. On the one hand, it is certainly fair to say that being enrolled in the “private option” is far better than remaining uninsured. We should also realize that even these compromise plans are just barely being passed in states like Arkansas. On the other hand, however, endless compromise may eventually make life even harder for the sick poor. As some have argued, the universal expansion of Medicaid might be only a matter of time: According to reporter Geoffrey Cowley, 24 states initially opted out after the original Medicaid bill was passed, a number that fell to two by 1970. Reactionary state governments may yet succumb to unrelenting political pressure and moral outrage.
But regardless of where we fall on political strategy, the implications of the private option seem unequivocal. They advance, in ways small and large, ideas that are at the center of the “consumer-driven” health policy revolution. The idea of true universal health care – with equal benefits and access for all, free at the point of care – is in retreat; neoliberal health care ideology, in contrast, remains ascendant in the age of Obamacare.
Join us in defending the truth before it’s too late
The future of independent journalism is uncertain, and the consequences of losing it are too grave to ignore. To ensure Truthout remains safe, strong, and free, we need to raise $43,000 in the next 6 days. Every dollar raised goes directly toward the costs of producing news you can trust.
Please give what you can — because by supporting us with a tax-deductible donation, you’re not just preserving a source of news, you’re helping to safeguard what’s left of our democracy.